What is glaucoma?
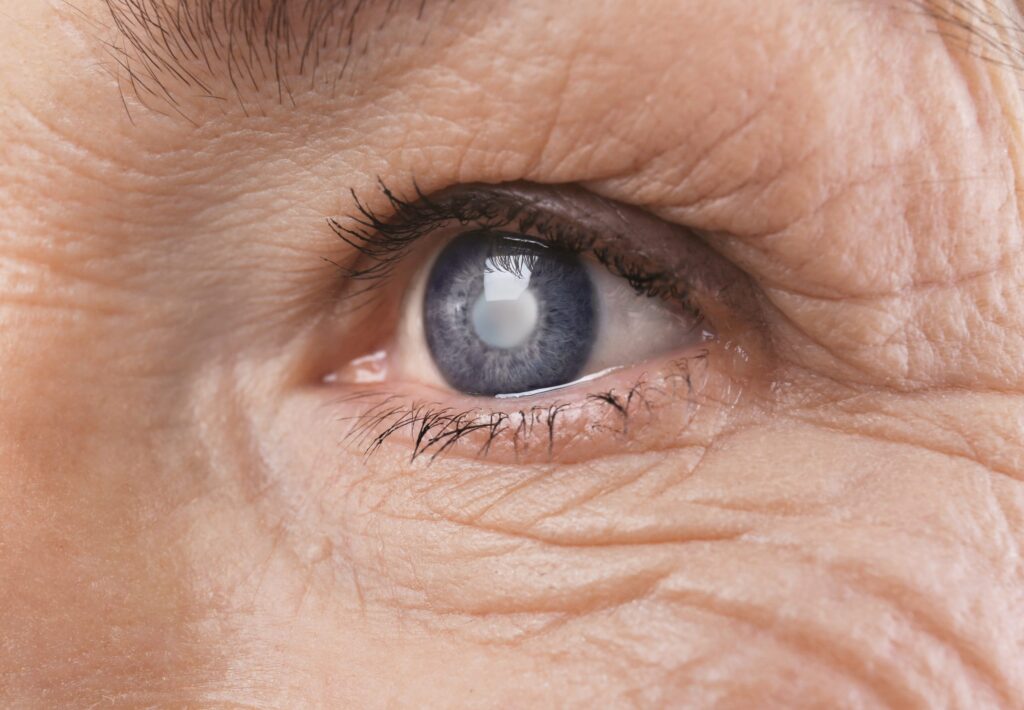
Glaucoma is a progressive eye disease that damages the optic nerve, often due to increased pressure within the eye. It is one of the leading causes of irreversible blindness worldwide. Glaucoma typically develops gradually and without noticeable symptoms, making it crucial to understand the disease and its impact on vision.
The condition predominantly affects older adults, but it can occur at any age. Early identification and management are vital to preventing severe vision loss. With advancements in medical research and treatment, many individuals with glaucoma can maintain their sight if they adhere to treatment protocols. Regular check-ups with an eye care professional are essential, as they can help monitor eye pressure and assess the health of the optic nerve, ensuring that any changes are detected promptly.
Furthermore, lifestyle factors such as diet, exercise, and managing systemic health conditions like diabetes and hypertension can play a significant role in the progression of glaucoma. A balanced diet rich in antioxidants, for instance, may support overall eye health, while regular physical activity can help maintain healthy intraocular pressure levels. Awareness of family history is also crucial, as genetic predisposition can increase the risk of developing this condition.
The science behind glaucoma
The eye functions similarly to a camera, with light entering through the cornea and being focused on the retina at the back of the eye. The optic nerve carries visual information from the retina to the brain, where it is interpreted as images. Glaucoma primarily affects this critical optic nerve, often caused by ocular hypertension, which arises from an imbalance in the production and drainage of aqueous humour, the fluid that fills the eye. Early awareness of the symptoms of glaucoma can aid in timely medical intervention, reducing the risk of further vision impairment. Understanding the common and less common symptoms is essential for recognising potential issues more effectively.
This increased pressure can lead to damage over time, particularly if it reaches elevated levels. However, it is essential to note that glaucoma can also occur with normal eye pressure, known as normal-tension glaucoma. Understanding these mechanisms can shed light on the importance of regular eye examinations for early detection. In addition to pressure levels, factors such as age, ethnicity, and existing health conditions can influence an individual’s risk profile, highlighting the need for tailored screening approaches.

Different types of glaucoma
Glaucoma is classified into several types, with the two most common being open-angle and angle-closure glaucoma. Open-angle glaucoma, the most prevalent form, occurs gradually and is painless, resulting in a slow loss of peripheral vision.
Angle-closure glaucoma, on the other hand, is much rarer and can occur suddenly, causing severe eye pain, nausea, and blurred vision. Other types include congenital glaucoma, which is present at birth, and secondary glaucoma, which can develop due to other medical conditions or injuries. Each type of glaucoma may require different treatment approaches, ranging from eye drops to surgical interventions, underscoring the importance of accurate diagnosis and personalised care. Additionally, ongoing research into new therapies and technologies continues to evolve, offering hope for improved management and outcomes for those affected by this complex condition.
Recognising the symptoms of glaucoma
A significant challenge with glaucoma is its insidious onset, often presenting no symptoms in the early stages. This lack of noticeable signs means many individuals may not be aware of their condition until considerable damage has occurred.
Common symptoms to look out for
Individuals at risk should be vigilant in observing any changes in vision. Common symptoms associated with glaucoma include gradual peripheral vision loss, often described as tunnel vision, difficulty adjusting to changes in lighting, and blurred vision.
In some cases, patients may experience halos around lights, indicating that pressure is impacting the optic nerve. Regular self-assessment and being attentive to these signs can be critical in seeking medical advice promptly. It is also advisable for individuals to undergo regular eye examinations, as these can help detect early signs of glaucoma even before symptoms become apparent. Optometrists can conduct tests to measure intraocular pressure and assess the health of the optic nerve, providing invaluable insights into one’s ocular health.
Click here to find about test for glaucoma.
Less common symptoms of glaucoma
While the above symptoms are more recognised, less common symptoms may also occur. These include eye pain, redness, headaches, and sudden vision changes. Angle-closure glaucoma can lead to acute symptoms, such as intense pain, nausea, and vomiting, necessitating immediate medical attention.
Individuals should not dismiss these symptoms, especially if they occur suddenly or dramatically disrupt vision. They warrant a prompt visit to an eye care professional for comprehensive evaluation. Furthermore, it is worth noting that certain risk factors, such as family history, age, and underlying health conditions like diabetes or hypertension, can increase the likelihood of developing glaucoma. Therefore, being proactive about eye health and discussing any concerns with a healthcare provider is essential for those who may be at higher risk. Regular monitoring and education about the condition can empower individuals to take charge of their visual health more effectively.
The importance of early detection
Early detection of glaucoma is paramount for effective management and preservation of vision. The longer the disease goes undiagnosed, the greater risk of irreversible optic nerve damage increases.
Understanding why early detection matters can motivate individuals to prioritise regular eye check-ups, even when asymptomatic. This proactive approach can lead to timely interventions that make a substantial difference in outcomes. Moreover, the psychological impact of knowing one’s eye health status can alleviate anxiety and uncertainty, empowering patients to take control of their health. Find more about psychological on https://psychology.missouri.edu/what-psychology
How early detection can help
Early detection allows healthcare professionals to initiate treatment before significant damage occurs. With appropriate management strategies, many patients can halt or slow the progression of the disease.
Continuous monitoring can guide adjustments to treatment plans based on individual responses, ensuring optimal care tailored to each patient’s needs. The inclusion of patient education about their condition also fosters better adherence to prescribed treatments. Furthermore, advancements in technology, such as optical coherence tomography (OCT), have enhanced the ability to detect subtle changes in the optic nerve, making it easier for practitioners to identify at-risk individuals early in the disease process.
The role of regular eye check-ups
Regular eye check-ups play a crucial role in early detection. Health professionals typically employ comprehensive examinations, including measuring intraocular pressure, assessing the optic nerve, and conducting visual field tests.
The recommendation is for individuals over 40 to have eye examinations every two years, or more frequently if they are at higher risk for glaucoma. Such proactive measures ensure any changes can be detected and managed efficiently. Additionally, those with a family history of glaucoma or other risk factors, such as diabetes or high blood pressure, should consider discussing their eye health with a specialist. By fostering a culture of regular eye care, communities can significantly reduce the prevalence of advanced glaucoma and its associated complications.
Treatment options for glaucoma
Once diagnosed, various treatment options are available to manage glaucoma effectively. The goal of treatment is to lower intraocular pressure and prevent further damage to the optic nerve.
Patients may need to explore different treatment pathways based on the type and severity of their condition. It is essential to understand these options to make informed decisions regarding personal health.
Medication and its effectiveness
Medications are the first line of defence against glaucoma. These typically come in the form of eye drops that help reduce intraocular pressure by either decreasing the production of aqueous humour or enhancing its drainage.
While effective for many, adherence to prescribed medication is vital for maintaining pressure control. Regular follow-ups and communication with an eye care professional will ensure that any side effects or ineffectiveness of treatments can be assessed and addressed. Furthermore, patients should be aware that some medications may take time to show results, and it is crucial to remain patient and consistent with the treatment regimen. In addition, lifestyle factors such as diet, exercise, and stress management can also play a role in overall eye health, and patients are encouraged to discuss these aspects with their healthcare provider.
Surgical treatments for glaucoma
If medications alone do not sufficiently control intraocular pressure, surgical options may be considered. Surgical treatments for glaucoma can include procedures such as trabeculectomy, where a small drainage hole is created in the eye to help fluid escape, or the implantation of drainage devices.
Other techniques, such as laser treatments, can also improve drainage and reduce intraocular pressure effectively. These surgical interventions can provide significant benefits, particularly in more advanced cases of glaucoma. It is important for patients to understand that while surgery can be highly effective, it does carry risks, including infection, bleeding, or even vision loss. Therefore, a thorough discussion with an ophthalmologist about the potential benefits and risks is essential before proceeding with any surgical options. Additionally, post-operative care and monitoring are crucial to ensure the best possible outcomes and to manage any complications that may arise during the recovery process. To learn more about infection click here.
Living with glaucoma
Living with glaucoma can present challenges, but understanding that the condition is manageable plays an essential role in maintaining a high quality of life. With the right treatment plan and lifestyle adjustments, individuals can adapt to their condition. Regular check-ups with an ophthalmologist are crucial, as they can monitor the progression of the disease and adjust treatments as necessary. Early detection and intervention can significantly reduce the risk of vision loss, making it imperative for patients to adhere to their scheduled appointments.
Support systems, including family and friends, along with mental health resources, can further aid in coping with the emotional aspects of dealing with a chronic illness. It is important for loved ones to be educated about glaucoma, as this understanding can foster a more supportive environment. Open conversations about the challenges faced can strengthen relationships and provide a sense of community, which is invaluable for emotional well-being.
Lifestyle changes to manage glaucoma
Making lifestyle changes can have a positive impact on managing glaucoma. These changes may include maintaining a healthy weight, exercising regularly, and following a balanced diet rich in fruits and vegetables. Incorporating foods high in omega-3 fatty acids, such as fish and flaxseeds, can also be beneficial, as some studies suggest they may support eye health. Furthermore, staying hydrated is essential, as proper hydration can help maintain intraocular pressure, which is crucial for glaucoma patients.
Additionally, avoiding smoking and limiting alcohol consumption are helpful strategies. Remember that any lifestyle adjustments should be discussed with a healthcare professional to ensure they align with the individual’s treatment plan. It’s also worth noting that some patients find mindfulness practices, such as yoga or meditation, to be beneficial in managing stress, which can have a positive effect on overall health and well-being.
Emotional and psychological support for glaucoma patients
Dealing with a chronic condition such as glaucoma can exert emotional and psychological strain on individuals. It’s vital for patients to seek emotional support from family, peer groups, or professional counselling services. Many patients may experience feelings of isolation or fear regarding their vision, and addressing these feelings openly can be a critical step towards emotional resilience. Engaging in activities that promote social interaction, such as joining clubs or participating in community events, can also help alleviate feelings of loneliness.
Engagement in support groups can provide comfort and understanding, connecting individuals facing similar experiences. These groups often share valuable insights and coping strategies that can empower patients to take an active role in their health management. Seeking psychological support enables patients to develop coping strategies to better manage the feelings of anxiety and uncertainty that may arise during their journey with glaucoma. Techniques such as cognitive behavioural therapy (CBT) have been shown to be effective in helping individuals reframe negative thoughts and enhance their overall outlook on life despite the challenges posed by their condition.