Welcome to Stomach Bloating Solutions
Finding Relief for Digestive Discomfort.
Are you struggling with stomach bloating? We’re here to help you find relief and regain comfort in your life.
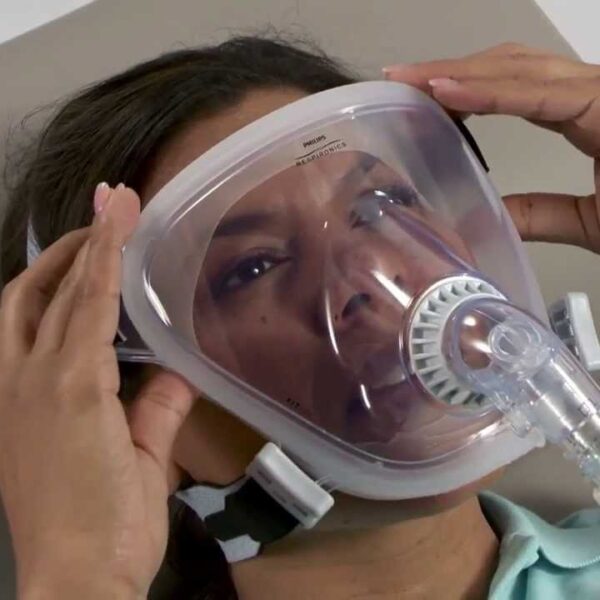
Explore our range of CPAP machines, masks, and accessories tailored to meet your needs. Whether you’re looking to manage sleep apnea or improve your digestive health with best cpap mask.
Discover effective solutions and personalized support at Stomach Bloating Solutions.


Our Company
Stomach Bloating Solutions
Welcome to Stomach Bloating Solutions, where we are dedicated to providing effective solutions for digestive discomfort and sleep apnea management. Our company is founded on the principles of compassion, expertise, and innovation to help individuals lead healthier lives.
I have been struggling with stomach bloating and sleep apnea for years, and finding Stomach Bloating Solutions was a game-changer for me. Their products are top-notch, but what really sets them apart is their exceptional customer service and genuine care for their customers’ well-being. Thanks to their guidance and support, I’ve been able to manage my symptoms more effectively and enjoy better sleep. I can’t recommend Stomach Bloating Solutions enough!
William M. Johnson
Our Values
At Stomach Bloating Solutions, we are guided by a set of core values that shape everything we do:
01.
Excellence
We are committed to excellence in every aspect of our business, from the quality of our products to the level of customer service we provide. We continuously strive to exceed expectations and set new standards of performance.
02.
Compassion
We approach our work with empathy and compassion, recognizing the challenges our customers face. We treat everyone with kindness, dignity, and respect, fostering a supportive and understanding environment.
03.
Innovation
We embrace innovation as a driving force behind progress. We stay at the forefront of advancements in digestive health and sleep technology, constantly seeking new solutions and improving existing ones to better serve our customers.
04.
Integrity
Integrity is at the heart of everything we do. We uphold the highest ethical standards in our interactions with customers, partners, and colleagues. Honesty, transparency, and accountability are the cornerstones of our business practices.
05.
Collaboration
We believe in the power of collaboration and teamwork. By working together internally and with our partners, we leverage our collective knowledge and expertise to deliver superior outcomes for our customers.
06.
Community
We are dedicated to building a strong and supportive community of individuals who share our commitment to health and wellness. We actively engage with our community, offering resources, support, and encouragement to help individuals achieve their health goals.

Our Products
Committed to Quality
Explore our comprehensive range of products designed to address digestive discomfort and sleep apnea:
CPAP Machines
Discover a variety of CPAP machines tailored to meet your specific needs and preferences. Our selection includes advanced models with innovative features to ensure optimal comfort and effectiveness.
CPAP Masks
Choose from a diverse array of CPAP masks designed for maximum comfort and performance. Whether you prefer nasal masks, full-face masks, or nasal pillow masks, we have options to suit every individual.
ResMed AirMini
Experience the convenience and portability of the ResMed AirMini, the world's smallest CPAP machine. Ideal for travel or everyday use, the AirMini delivers effective therapy in a compact and lightweight design.
ResMed AirSense 10
Explore the ResMed AirSense 10 series, renowned for its advanced features and user-friendly interface. With integrated humidification and smart technology, the AirSense 10 ensures a comfortable and personalized therapy experience.
Our Blogs
Explore our informative blogs covering a wide range of topics related to digestive health, sleep apnea, CPAP therapy, and more:
Our Purpose
Empowering Healthier Lives
At Stomach Bloating Solutions, our purpose is clear: to empower individuals to live healthier, happier lives by providing effective solutions for digestive discomfort and sleep apnea.
What Drives Us
We understand the profound impact that digestive issues and sleep disturbances can have on overall well-being. That’s why we are committed to offering more than just products — we provide support, guidance, and education to help our customers take control of their health and improve their quality of life.